A collection of all the microorganisms (bacteria, viruses and fungi) is known as the microbiome. Each person has a unique microbiome community found on and inside the body, which in most cases protects against infections.
Although the microbiome is unique to individuals, generally the microbial composition is similar amongst healthy individuals with microorganisms belonging to the phyla Firmicutes (recently renamed Bacillota) and Bacteroidetes in the majority. The Firmicutes are Gram-positive bacteria and include the genera Bacillus, Clostridium, Enterococcus, and Lactobacillus, while Bacteroidetes are Gram-negative, obligate anaerobic bacteria such as Bacteroides vulgatus, B. fragilis, and B. pyogenes.
Join our WhatsApp ChannelIt is widely known that bacterial colonisation of the gut is essential for the development and maturation of both the central nervous system and the enteric nervous system (i.e. the gut nervous system with its array of neurotransmitters).
A robust gut microbiota is important to the body’s general wellbeing. The gut-brain axis or crosstalk is an important but complex bidirectional communication system between the brain and the gut. It monitors and integrates gut functions and links these to the emotional and cognitive part of the brain relating to intestinal functions and mechanisms such as immune activation and intestinal permeability.
In the centre of this crosstalk between the brain and the gut is the gut microbiota. Gut microbiota signalling to the brain and from the brain to gut microbiota occurs by means of neural, endocrine, and immune links.
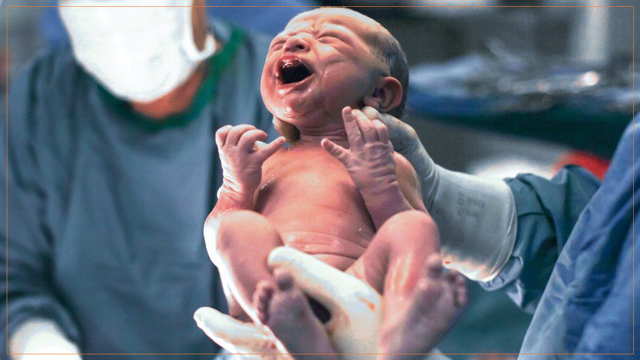
Birth by caesarean section disturbs natural microbiota colonisation and development by preventing maternal transmission of gut bacteria to the newborn. Babies born through caesarean sections are disadvantaged in acquiring a beneficial microbiome to protect them while the immune system is still developing. This might mean that they are predisposed to more infections compared with naturally born babies. For example, a study conducted between 1982 and 2010 showed that C-section babies have an increased risk of developing inflammatory bowel disease, rheumatoid arthritis, celiac disease (i.e. gluten intolerance autoimmune disorder), and type 1 diabetes.
Naturally born babies are coated with their mother’s vaginal fluids as they pass through the vagina during birth. This helps in the development of the baby’s microbiome and immune function, thus, lowering the risk of infections. Vaginally delivered babies acquire microbial communities akin to those found in their mother’s vagina, mainly Lactobacillus, Escherichia, and Bacteroides while C-section babies tend to have higher levels of bacteria that are commonly found in the hospital environment such as species of Staphylococcus, Enterococcus, and Klebsiella. Such disparity in microbiome composition is due to the fact that the succession of the microbiome from the mother’s birth canal is disrupted by caesarean section resulting in increased infection risks when compared with normal vaginal delivery.
A study published in the July 2023 issue of the journal, Cell Host & Microbe, by Lepeng Zhou and coworkers, showed that vaginal seeding or vaginal microbiota transfer (VMT) may improve the development of microbiome of the newborn C-section babies. This was done by simply swabbing C-section babies with their mother’s vaginal fluid soon after birth.
Zhou and coworkers selected 68 women who were due for caesarean births and screened them against infections that could be potentially harmful to the babies. The babies were randomly smeared with their mother’s vaginal fluid, and the rest were smeared with saline solution, as control. An additional 33 pregnant women scheduled for C-section were also included as reference groups for comparison. C-section babies from this latter group were not swabbed.
Both groups of babies (vaginal fluid- and saline solution-swabbed babies, respectively), did not show any serious health issues, and both have mild fevers and skin conditions. However, it was observed that C-section babies who were swabbed with their mother’s vaginal fluid soon after birth had improved neurodevelopmental skills like communication, movement, problem-solving, social and personal skills, which include reaching out for toys and smiling at their reflections in a mirror, than those who were swabbed with only saline solution or not swabbed at all.
Further, vaginal seeding of C-section babies soon after birth significantly improved the maturation of microorganisms found in the gut (ie gut microbiota) within 42 days after birth, and also regulated the quantities of some faecal metabolites and metabolic functions that include carbohydrates, energy, and amino acid metabolisms.
Faecal microbiota transplantation (FMT), a technology we have discussed twice before in this column, is an emerging technology. The principle is to use microorganisms found in the guts of healthy donors to treat diseases. The process requires the introduction of healthy donor faeces in the form of pills into the gut of a patient. Alternatively, screened raw faeces can be introduced into the patient by enema or gavage (ie feeding a patient donor faecal sample by inserting a small tubing through the nose or mouth down to the stomach).
READ ALSO: Health Risks Of Microwaving Food In Plastics
Faecal microbiota transplantation has found use not only in treating many medical conditions, including Clostridium difficile infections and advanced skin cancer but also it has been used to introduce gut microbiomes of the mother into C-section babies. Through this process, the mother’s diluted faecal sample is fed to the baby, resulting in the introduction of microbiomes that closely mirror those in babies who were born vaginally.
Thus, C-section babies could have their gut microbiota improved by either swabbing them with their mother’s vaginal fluid or giving them a diluted faecal sample of their mother mixed with breast milk.
Given the importance of the gut microbiota in the metabolic and physiological functions of the body, including regulating the body’s homeostasis (temperature and fluid balance), one wouldn’t be surprised if, in the next few years, we see commercialised vaginal fluids for C-section babies being sold over the counter. Until then, if you must resort to do-it-yourself (DIY), please make sure it is done under medical supervision so that the mother can be screened against harmful bacteria that may endanger the health of the baby.














Follow Us