In the good old days, piling on the pounds was regarded as evidence of good living, but nowadays, society dictates that thinness is the new normal. In fact, anorexia is considered even more fashionable.
Last year WHO estimated the number of people that are obese to be more than a billion and the number is continuing to increase. The people that pile up the pounds are in most cases predisposed to health issues, such as type 2 diabetes, heart disease, stroke and some types of cancers.
Obesity is often a stigma for sloth and gluttony and therefore, is regarded as a lifestyle choice. But obesity in most cases is genetic, especially when coupled with environmental factors, poor dieting, and lack of physical activity.
Is obesity therefore, a disease? The jury is still out there on that score. While some people recognise obesity as a complex disease that predisposes people to other diseases, others recognise the fact that one can be obese and still be healthy. In other words, obesity is not always associated with negative health effects. Some countries classify and treat obesity as a disease, while others don’t, for example, the USA treats obesity as a disease but the UK as of 2019, don’t.
Healthier lifestyle and physical exercises are usually the antidotes to obesity. But not everybody responds or is privileged to indulge in such luxuries. For such people, bariatric surgery offers a solution. However, bariatric surgery is not slam dung for obesity, it does have its pros and cons.
But if you are afraid to go under the knife, help is now at hand. You can lose weight by simply taking medication. No more dragging yourself to the gym and running the gauntlet of supercilious smiles from the skinnies or stinting yourself of those delicious foods and ice creams.
Hurray! But not so fast, amigo. The medication comes with a cost. It stops you from getting hungry! Typical, I hear you groan in frustration.
Ideally, reducing the overall bodyweight to about 10% can improve (and in some cases reverse) many of the obesity associated issues. The new arrays of anti-obesity medications generally act by controlling appetite through various mechanisms such as slowing gastrointestinal transit and reducing glucose levels.
READ ALSO: 10 Healthy Ways Of Reducing Risk Of Breast Cancer
The search for anti-obesity drugs was boosted in 1994 when Dr Jeffrey Friedman at The Rockefeller University, USA, discovered that giving a fat tissue hormone supplement called leptin, to mice that lacked it, reduced their hunger and bodyweight. This is because leptin regulates food intake through binding to the leptin receptor, and mutations in the leptin receptor have been known to cause excessive hunger and weight gain, as seen in monogenic childhood obesity.
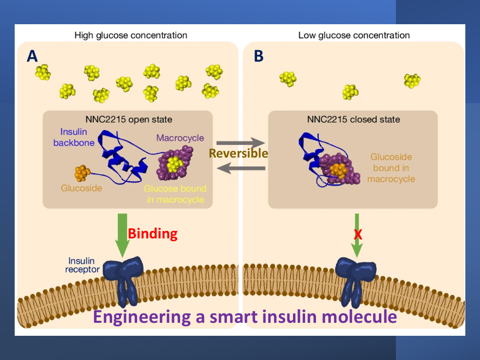
Then came the discovery of another hormone called GLP-1 (glucagon-like peptide 1). This hormone increases the production of insulin while reducing blood sugar – a direct opposite effect of Type 2 diabetes! Consequently, drugs that mimicked GLP-1 were approved for the treatment of Type 2 diabetes.
And yet another surprise, weight reduction was observed in obesity patients who participated in the clinical trials of these GLP-1-based drugs. The reason for this was that GLP-1 affects brain receptors responsible for appetite as well as receptors in the gut that slow digestion. Scientists quickly connected the dots and clinical trials of these anti-diabetic drugs were conducted for weight loss.
Based on these trials, one such drug called Liraglutide, emerged. The drug had the modest capacity to reduce bodyweight by about 8%. A modified version of liraglutide called Semaglutide underwent a Phase 3 clinical trial in early 2021. Weekly injections of the drug, semaglutide, results in 15% average loss of bodyweight after 16 months’ treatment regime. The drug’s improved efficacy is suspected to be due to its ability to remain intact and active in the body longer than its predecessor. Semaglutide is also suspected of permeating brain regions associated with regulating appetite more efficiently than liraglutide. The drug is now approved for treatment of obesity.
Glucose-dependent insulinotropic polypeptide, (GIP), also known as gastric inhibitory polypeptide, is a hormone that plays a role in food digestion. Upon release from the small intestine following food intake, GIP stimulates insulin secretion from the pancreas depending on blood glucose levels. Insulin controls the storage of nutrients contained in foods in the liver, fat and muscle.
Glucose-dependent insulinotropic polypeptide is also involved in slowing the emptying of food from the stomach. This process directly affects the rate at which fats in food are broken down and stored. People with type 2 diabetes secretes little quantities of GIP, and even when administered with naturally occurring GIP doses, insulin secretion in type 2 diabetics remains very low.
A new wonder anti-diabetic drug called Tirzepatide works by activating GLP-1 receptor while mimicking the GIP hormone to cause weight loss. The drug was approved last year for type 2 diabetes but is found to reduce bodyweight by an average of 21%, almost comparable to those achieved through surgical bariatrics! Eli Lilly, Indianapolis, USA, who developed tirzepatide, plans to seek for approval of the drug for treatment of obesity pending a successful outcome of their second Phase 3 clinical trial scheduled to end by this April.
The pharmacological strategy to controlling obesity has given rise to a slew of approaches targeting gut hormones involved in appetite. Controlling one’s weight will soon be just a matter of popping pills. But the pills are not cheap, monthly intake of pills to keep your bodyweight down could set you back by a $1000!
Still, if you can afford it, it is a small price to pay in exchange for those delicious foods and mouthwatering chocolates and ice creams – no pun intended to people whose bodies are naturally predisposed to obesity.













Are the drugs free from side effects?