In 2021 a new drug was approved by the US Food and Drug Administration for the treatment of obesity. The drug by the generic name of Semaglutide is popularly known by its trade name Wegovy. It was said to reduce body weight by at least 20% for one-third of clinical trial participants and is also prescribed for the treatment of type 2 diabetes under the brand name Ozempic.
In 2022 another drug called Tirzepatide, was approved. Tirzepatide, which sold under the name Mounjaro, is similar to Semaglutide but with a more impressive clinical trial result. The drug although originally approved for the treatment of type 2 diabetes, is also prescribed for the treatment of obesity.
Join our WhatsApp ChannelCombined, both drugs and similar ones are revolutionising the treatment of obesity and type 2 diabetes and are acquiring a social media status many drugs would love to kill for – pardon the pun. To add to their social media status, the drugs have acquired a new reputation for their “welcome or unwelcome” side effect – they are reputed to cause unplanned pregnancies!
The social media claims range from some women getting pregnant despite using birth-control pills, to medically diagnosed infertile women being able to conceive after a regimen of the drugs.
READ ALSO: Anti-Obesity Drugs Winning The War On Fat
Normally, most scientific minds do not take social media stories and claims seriously, but the excitement these drugs have generated in social media platforms is enough to cause scientists to take interest and are now beginning to unravel the mysteries surrounding the unplanned pregnancy claims associated with the drugs.
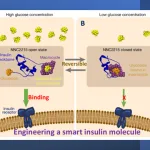
Glucagon is a peptide hormone secreted in the pancreas. The peptide hormone is an antithesis of the insulin hormone. While it regulates blood sugar levels by increasing glucose concentration in the blood, insulin on the other hand reduces blood sugar levels. Another hormone called glucagon-like peptide 1 (GLP-1) is produced in the intestine and has the metabolic effect of stimulating insulin secretion from the pancreas in response to high blood sugar levels. In other words, GLP-1 hormone exerts a glucose-dependent inhibition of glucagon secretion. The hormone also regulates appetite by inhibiting food intake through tricking the brain into thinking that your stomach is full. According to the latest “first release” publication in the journal, Science, by Kyu Kim and coworkers, the part of the brain involved in this process is the dorsomedial hypothalamus (DMH). The neurones of DMH have GLP-1 receptors for docking of GLP-1. Thus, GLP-1 is able to directly act on this part of the brain to produce a feeling of fullness (or satiation) even when you have eaten only little or no food at all.
Reports abound of the cardio- and neuroprotective effects of the GLP-1 hormone as well as its involvement in learning and memory, and in lowering inflammation in the liver, kidneys and heart. It has even been reported to reduce inflammation in the brain, which offers hope that one day GLP-1 analogues modified biochemically for enhanced potency and sustained action, could be used for the treatment of Parkinson’s and Alzheimer’s. In fact, an article which appeared in the April 2024 edition of the New England Journal of Medicine shows that a GLP-1 receptor agonist called Lixisenatide slows the symptoms of Parkinson’s, including the progressive loss of motor control.
GLP-1 hormone has a pleiotropic influence on the body, some of which have been mentioned above. Currently two of these are being commercially exploited. Its ability to stimulate the production of insulin in order to control blood sugar levels has made it a commercial success for the treatment of type 2 diabetes. While its appetite-regulating capabilities have made it an ideal weight loss medication. The two drugs, Semaglutide and Tirzepatide, and other variants, are synthetic versions of GLP-1. Though the drugs mimic GLP-1 by binding to the same receptor, their degradation is very slow compared with the natural hormone. This means that they are able to suppress appetite for food much longer.
Hormonal imbalances lead to menstrual cycle disruptions, a problem often experienced by obese women. The hypothesis is that taking GLP-1 drugs for weight reduction could also restore regular ovulation in obese women. Thus, obese women on a course of GLP-1 drugs can lose weight as well as regain their ovulation.
Synthetic GLP-1 drugs slow the rate at which food and medications empty out of the stomach and into the small intestine. Oral contraceptives are absorbed into the bloodstream from the small intestine. In effect, GLP-1 drugs influence the concentration of drugs available for absorption into the bloodstream by slowing the rate at which the drugs are emptied into the stomach. In fact, Tirzepatide (ie Mounjaro) has been shown to reduce the concentration of contraceptives in the blood by as much as 66% after just a single dose, making the pregnancy-preventative action of contraceptives redundant.
A report published in the November 2015 issue of the journal, Endocrinology, showed that GLP-1 has a regulatory impact on the reproductive system by increasing the production of luteinising hormone. This hormone triggers ovulation in rats and humans. When GLP-1 was given by Intracerebroventricular injection (ie icv) to female rats, two things happened: an increase in the number of foetuses implanted and an increase in the number of pups born.
Evidence for the role of anti-obesity and diabetes drugs in enhancing fertility is certainly coming thick and fast. Polycystic ovary syndrome (PCOS) disrupts the function of the ovary leading to difficulty in getting pregnant. An estimated 5% to 20% of women worldwide experience this condition, and the symptoms include irregular periods or non at all, growing excessive facial hair, and difficulty getting pregnant. The cause for PCOS is not exactly known but genetics is a big suspect. Obesity may also be a contributory factor as well as having high levels of a male hormone called androgens, which prevent egg release from the ovary. Prevention of the ovary from releasing eggs leads to irregular menstrual cycles. While there is no known cure for PCOS, the symptoms of excessive hair growth, obesity and irregular menstruation, can be medically managed.
Yun and coworkers writing in the May 2024 edition of the journal, Nature Metabolism, presented evidence to show that Bacteroides vulgatus, a gut bacterium, may present symptoms of PCOS through the process of metabolising an amino acid called arginine to produce agmatine. Agmatine through its activation of the bile acid receptor (or farnesoid X receptor, FXR) pathway is able to inhibit the secretion of GLP-1. This inhibitory action leads to insulin resistance and ovarian dysfunction. Liraglutide is a GLP-1 receptor agonist sold commercially as Saxenda, which is prescribed for weight loss, and as Victoza for type 2 diabetes. When female mice were given Liraglutide, the ovarian dysfunction was resolved, and the female mice ovulated once again.
Taken together, there are overwhelming evidence to suggest that synthetic GLP-1 drugs used for treating obesity and diabetes may play a role in promoting pregnancy by limiting the absorption of contraceptives into the bloodstream and secondly, by restoring ovulation. But the exact mechanism/s is yet to be convincingly established. I guess a rule of thumb applies here: if it looks like a duck, swims like a duck, and quacks like a duck, then it probably is a duck.
However, before embarking on a course of GLP-1 drug to manage weight gain or to get pregnant, it is worth knowing that like every other drugs, GLP-1 drugs do have some unpleasant side effects, which include nausea, constipation (caused by delayed digestion and absorption of food), muscle loss, and pancreatitis (i.e. an inflammation of the pancreas). GLP-1 medication can also result in gastroparesis, which is a condition that slows or stops the movement of food from the stomach into the intestine.

















Follow Us