Insulin is an indispensable hormone needed to regulate sugar levels in the body. Type 1 diabetes occurs when the immune system attacks and destroys insulin-producing cells in the pancreas. And in type 2 diabetes, the pancreas produces limited amount of insulin, or the body cells become insensitive to insulin.
Food digestion results in the absorption of nutrients into the bloodstream causing a spike in blood sugar levels. Insulin produced in the pancreas extracts the glucose into cells for conversion into energy or storage in the form of glycogen in the liver, muscles, brain, and other tissues. Insulin binding to receptors on the liver prevents it from producing glucose. In an enzymic process called glycogenolysis, conversion of glycogen back to glucose occurs when the body experiences low levels of glucose or requires a burst of energy.
Join our WhatsApp ChannelHowever, regulating blood glucose using insulin is difficult due to fluctuations in blood glucose levels, which arise from a host of factors, namely, the type of, quantity, and frequency of food eaten, intense or too little or lack of exercise, illness, and the level of individual sensitivity to insulin. Too much insulin gives rise to low blood glucose or hypoglycaemia characterised by confusion, dizziness, coma, or death. And too little insulin results in hyperglycaemia or high blood glucose, characterised by thirst, increased frequency to urinate, tiredness, blurred vision, nerve damage, etc. Therefore, fine-tuning insulin doses is of immense importance in diabetes management.
To effectively control blood sugar levels, scientists over the years have been trying to create insulin molecules that can react to differing levels of blood glucose. One approach to managing high blood glucose levels in type 1 diabetes is to inject insulin under the skin (subcutaneous injection) several times a day, to lower blood glucose through uptake by fat and muscle tissues, and prevention of glucose synthesis by the liver. But this approach has a potential disadvantage in that it is not reversible. The injected insulin is still active so that even when the level of glucose returns to normal, the insulin action continues resulting in the drastic reduction of blood glucose and tilting the scale towards hypoglycaemia!
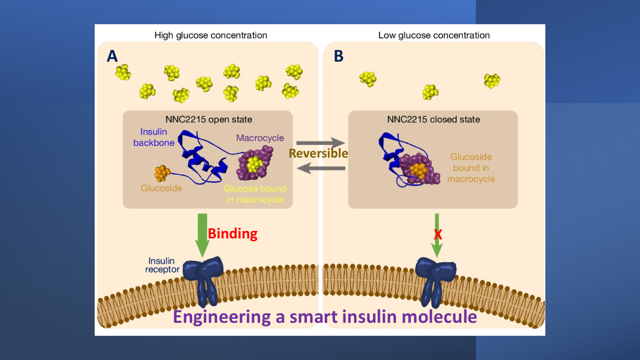
Rita Slaaby (the corresponding author) and coworkers reported in the October 2024 issue of the journal, Nature, the design of an artificial smart insulin that switches itself on and off in response to cues from blood glucose levels. The design and the mechanism of glucose control are as shown in the figure fronting this article.
The smart insulin molecule called NNC2215, has a two-part glucose-sensitive switch, comprising a ring-shaped macrocycle conjugated to a glucoside, a molecule derived from glucose. When blood glucose is high, the NNC2215 structure is in an open, active state (Figure A) and the glucose displaces the glucoside, causing the modified insulin to bind to the insulin receptor and in the process enables it to carry out its biological functions. But when blood glucose is low, the insulin structure is in a closed, inactive state with the glucoside binding to the NNC2215 ring cavity (Figure B).
The proof of the pudding is in the eating. The ability of the modified smart insulin to activate the insulin signalling pathway was trialled in rats and pigs. The result of the test showed that the modified insulin has the same effects as natural human insulin with no drop to the life-threatening levels common in insulin injections, thus proving the ability of the engineered smart insulin to respond to glucose fluctuations.
One of the problems faced by diabetics is the daily adjustment of insulin doses to account for fluctuations in blood glucose due to lifestyle factors, illness, etc. Glucose levels could drop dangerously low during the night leading to hypoglycaemia. To avoid such a drop in blood glucose, therefore, people tend to have the barest dose of insulin before going to bed. But this might give rise to insufficient insulin to control a rise in glucose level from nocturnal production of glucose by the liver and the resultant risk of hyperglycaemia.
Engineered glucose-induced biologics such as NNC2215 could be of use in circumventing blood glucose fluctuations and protect against hypoglycaemia, especially when combined with smaller doses of insulin at mealtime. This removes the risk of fast-acting insulin inducing hypoglycaemia as well as allows for tighter control of blood glucose levels.
READ ALSO: Diabetes Patients Groan As Monthly Medication Rises To N150,000
This study adds to many other interesting concepts relating to genetically engineered insulin molecules, including the long-acting insulins currently in use to control diabetes. It would be interesting to see the data when and if this molecule undergoes clinical trials with a view to adding it to the arsenal of drugs for control of diabetes.